Kidney Disease
The existing human and animal literature suggest that Klotho may be a promising biomarker for kidney disease and its symptoms. Future clinical studies should evaluate the safety and efficacy of Klotho therapy in CKD and AKI patients.
Klotho & Kidney Disease
Clinical and pre-clinical studies have demonstrated significant reductions in Klotho levels following CKD and AKI. In CKD patients, low circulating Klotho levels are associated with a more severe renal impairment. Increased methylation of the Klotho promoter has been evidenced in the diseased kidney and PBMC. This epigenetic alteration is one of the contributors to decreased Klotho levels in CKD patients. Klotho levels are also linked to electrolytes balance in CKD patients. In animal models, treatment with recombinant Klotho protein or plasmid significantly increases circulating and renal Klotho levels leading to a significant reduction in kidney pathology and an improvement in kidney function following CKD. Klotho exerts its beneficial effects on the diseased kidney by promoting nephroprotection and cell regeneration and by decreasing inflammation and renal fibrosis.
Overall, the existing human and animal literature suggest that Klotho may be a promising biomarker for kidney disease and its symptoms. Future clinical studies should evaluate the safety and efficacy of Klotho therapy in CKD and AKI patients.
Chronic Kidney Disease
Chronic kidney disease (CKD) is a life-threatening renal condition characterized by the progressive loss of kidney function. During its initial stages, the disease often goes undiagnosed and it is not until stage four or five when kidney damage reaches severe levels that patients seek medical help. Currently, there is no treatment for CKD.
According to the Centers for Disease Control and Prevention (CDC) there are about 37 million people in the U.S. (15% of the adult population) living with CKD. About 48% of people with reduced kidney function that are not on dialysis are not aware of having CKD. Advancing age is one of the most common risk factors for CKD and the majority of CKD patients are 65 years of age or older. Women are more susceptible than men to develop CKD and the disease is also more common in non-Hispanic blacks, than in non-Hispanic whites or non-Hispanic Asians. About 14% of the Hispanic population is estimated to have CKD.

Individuals with CKD can experience a variety of symptoms such as central nervous system (CNS) disorders, anemia, gastrointestinal tract & skin problems, endocrine dysregulation, cardiovascular disease, neuropathy, bone & muscle disease, and renal dysfunction. Multiple factors can increase the risk of developing CKD such as underlying kidney disease, genetic factors, and other health and lifestyle choices.
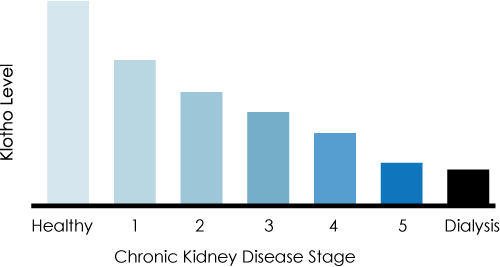
Decreased Klotho and Chronic Kidney Disease
The level of Klotho in the blood has been shown to decline as the stage of kidney disease increases. Humans on dialysis show dramatically lower levels of Klotho than healthy individuals.
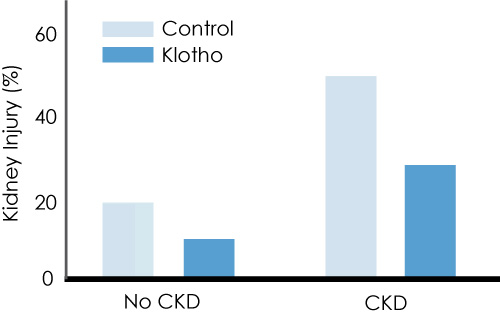
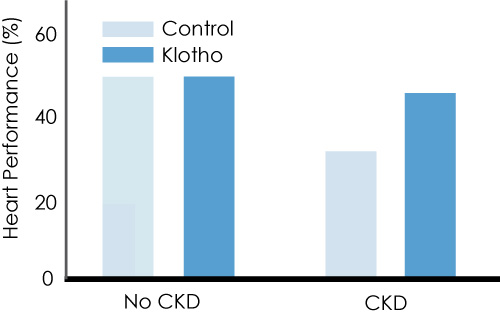
Klotho injections in animals slow the progression of kidney disfunction in chronic kidney disease (CKD) and for acute kidney injury (AKI) reduce the severity while promoting healing.
Injections Slow CKD and Adverse Cardiac Effects
In mice with chronic kidney disease, multiple injections of Klotho resulted in significantly less kidney and heart damage.
Acute Kidney Injury
Acute kidney injury (AKI) previously called acute renal failure (ARF), is a renal condition characterized by a sudden kidney failure occurring within hours to days. Multiple pre-renal, renal, and post-renal factors can lead to the occurrence of AKI and it currently has no cure.
AKI can affect other organs due to increases in:
- Uremic toxins
- Acid/base imbalance
- Electrolytes imbalance
- Inflammation
- Oxidative stress
- Neuro-hormonal dysfunction

AKI can cause end-stage renal disease (ESRD) directly and increase the risk of developing incident CKD and worsening of underlying CKD. In addition, the severity, duration, and frequency of a patient’s AKI can be a good predicator of their outcome. How are the two related? CKD is an important risk factor for the body’s future development of AKI and experimental data supports a relationship between the two. Studies have shown that patients who sustain multiple episodes of AKI as compared with a single episode of AKI have a higher likelihood of CKD progression. In a cohort of U.S. Veterans with diabetes (Thakar et al., 2011), those who had experienced two or more episodes of AKI were found more likely to progress to stage 4 CKD than patients who experience only one episode of AKI.
Studies on Klotho
Klotho is a single-pass transmembrane protein that is highly expressed in the kidney, brain, blood, and urine. This protein hormone is associated with a long, healthy life including healthy kidney function (Kuro-o et al., 1997).
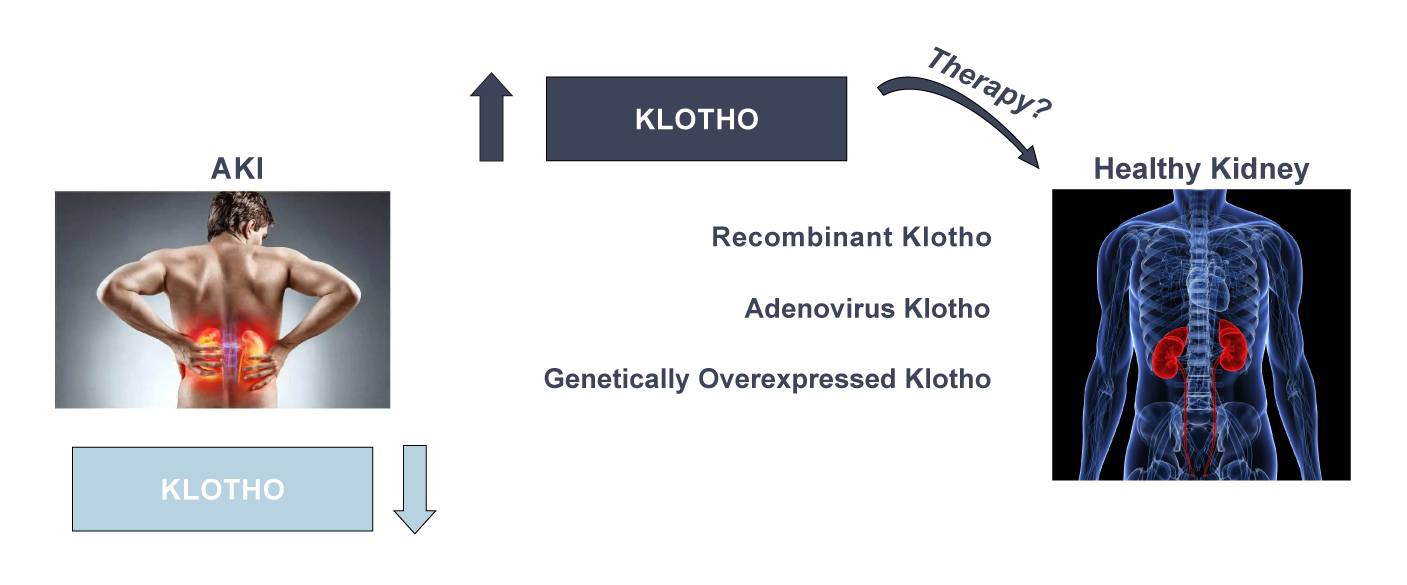
Clinical and preclinical studies have linked Klotho to kidney disease. Specifically, reduced Klotho levels have been evidenced in human patients with AKI as well as in animal models of the disease (Moreno et al., 2011). AKI patients with low circulating Klotho levels present more severe kidney dysfunction and poor outcome (Liu et al., 2015; Seo et al., 2015). In animal models, Klotho deficiency exacerbates kidney damage and dysfunction (Hu et al.,2010; Panesso et al., 2014). Treatment with a recombinant Klotho protein or adenovirus improves kidney pathology and function (Sugiura et al., 2005, 2010; Qian et al., 2018; Chen et al., 2018). Similarly, transgenic mice overexpressing Klotho protein show significantly less kidney damage and better recovery of kidney function following experimental AKI (Hu et al., 2010; Panesso et al., 2014). The cellular and molecular mechanisms mediating the reported Klotho effects on the injured kidney are related to the pro-survival and anti-fibrotic functions of this protein (Sugiura et al., 2010; Panesso et al., 2014; Qian et al., 2018; Chen et al., 2018).
Significantly Reduced Kidney Damage
Studies have shown that a single Klotho injection in animals shortly after AKI significantly reduced kidney damage vs. controls, as measured by levels of creatinine (lower is better). The result: reduced kidney damage and more complete recovery.
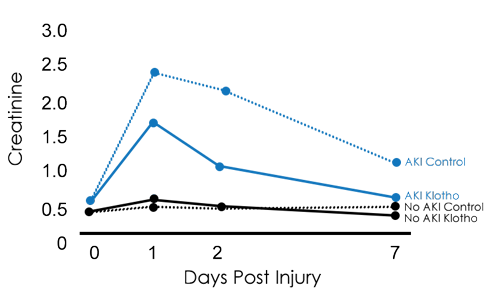
To investigate different pathophysiological pathways known to be involved in the pathogenesis of AKI, various animal models have been developed in mice and rats. All these models have given robust findings in mice and rats. Specifically, Klotho levels have been found to consistently decrease with AKI and Klotho treatment has been shown to rescue cell death in the injured kidney and promote functional recovery. These findings indicate that AKI-induced downregulation of renal Klotho is a general phenomenon following acute kidney insults such as ischemia, oxidative stress, and exposure to nephrotoxins and Klotho-based therapeutics may represent a new cure for AKI.
There have also been similar findings in relation to chronic kidney disease. Klotho levels decrease with CKD progression in CKD patients and animal models of CKD (Khodeir et al., 2019). Reduced Klotho levels are associated with more severe kidney damage in CKD patients (Akimoto et al., 2012), and increased methylation of the Klotho promoter in the kidney and peripheral blood mononuclear cells (PBMC) helps decrease levels of Klotho in CKD patients (Chen et al., 2013). Klotho is also dependent on electrolytes balance and FGF23 levels in CKD patients (Khodeir et al., 2019). These clinical findings have been confirmed in different animal models of CKD (Piao et al., 2013).
Learn More About Us
Careers
We offer careers in a range of disciplines such as bioengineering and chemistry. Apply today.